– What is pain?
The definition of pain has changed many times. It’s officially now sounds like this: “it is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or similar to such an experience.” See how many reservations there are: it says both about the subjectivity of the perception of pain, and about the fact that it may not have a real source.
These are all the fundamental points that were not taken into account before: “Does it hurt? It just seems this way to you!” Or simply: “Be patient.”
How and where is pain formed?
– Appeared not too long ago pain neuromatrix theory. According to her, all our reactions to external stimuli are laid down from birth.
Burns, blows and other sensations from the periphery are just triggers that contribute to the activation of this system. It hurts not only the finger that you pressed, it also “hurts” in the central nervous system.
Although the neuromatrix is genetically predetermined, its individual architecture is already being refined throughout life.
This is influenced by the person’s level of anxiety, past experience and awareness, auditory and visual stimuli at the time of the pain signal.
Further more. The brain can not only perceive incoming impulses, but also generate them itself. Remember the big push-button phones that vibrated a lot? Leaving the “pipe” at home, we could feel this vibration in our pocket all day long. This is an everyday example of how the brain generates pain perception, even if there are no signals from the periphery.
– Vibration, tickling, itching, cold – is it still pain?
“There are various receptors in the skin: some react to temperature, others to various types of mechanical touch, and so on. Absolutely any contact with the skin is an external stimulus, which is then interpreted by the brain.
This is how our perception of pain is formed (pain perception):
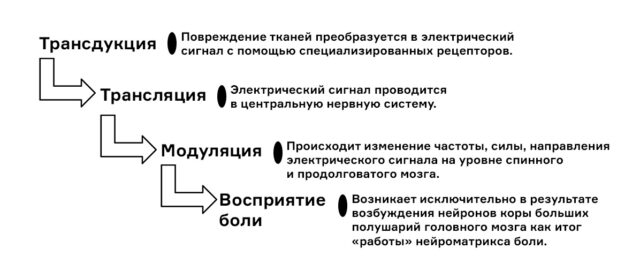
The whole process takes a fraction of a second. Sometimes you can even notice it: you burned yourself on the iron, but felt it only after a moment. The fact is that during a burn, type C nerve fibers react, in which the signal transmission speed is low, 2-3 m / s. For comparison: other fibers of skin receptors deliver a signal at a speed of up to 45 m/s.
Is there really a pain threshold?
The pain threshold is the level of irritation of the nervous system at which a person begins to feel pain. It exists and is different for everyone. There are people who, even when stroking or tickling, become extremely unpleasant. And there are those who will cut their hand with a knife and not notice. This does not mean that the first ones are sissies and simulators, they just have such a perception, and most importantly, they really hurt.
In order to somehow objectify all these emotional experiences, there are questionnairesused by algologists* in their work.
* There is no medical specialty “doctor-algologist” in Russia yet. Pain is treated by neurologists, anesthesiologists, and neurosurgeons.

Is it true that some people don’t feel pain at all?
– Congenital insensitivity to pain (CIP) is medically classified as peripheral neuropathy. In fact, this is an injury or disease that has led to damage to nerve cells. Such a rare condition deprives the ability to feel pain. As a result, pain stimulation never reaches the brain. There is nothing good in this: for example, such a person will not feel appendicitis and then peritonitis, then sepsis and even death.
– At the household level, pain is divided into dull, cutting, aching. How about science?
– The classification of pain in algology is completely different and depends on the mechanism of formation.
- nociceptive pain: associated with damage to any organ, joint, etc. Cut yourself – it hurts, broke your arm – it hurts.
- neuropathic pain: caused by some kind of interaction with the nerve. She has completely different characteristics: a tingling sensation, goosebumps, numbness. We experience neuropathic pain if we sit out our leg or bump our elbows. Also, this pain is well known to those who suffer from intervertebral hernias (radiculopathy).
- dysfunctional pain: occurs due to impaired perception. It may not have a source, but the brain will generate a pain impulse – by mistake or out of habit (if the stimulus was there for a long time, and then disappeared). A good example is phantom pain after amputation of a limb.
According to the duration, the pain is divided into acute and chronic. Acute pain – up to three months. Chronic – one that lasts more than three months. During this time, a dominant is formed in the central nervous system, which begins to send feedback: “I have must hurt and it will get sick”.
That is why tolerating pain is harmful. The longer you endure, the greater the likelihood of central sensitization of pain. That is, the excitability of sensory neurons increases, and ordinary, “normal” in intensity stimuli begin to be perceived as painful.
Can depression start from prolonged pain?
— Against the background of chronic pain syndrome, there is indeed a decrease in the level of serotonin and dopamine – “hormones of joy and pleasure”. But cause-and-effect relationships are different.
- There is depression that develops because of pain: a person suffers for so long that he loses his taste for life.
- There is depression, already against the background of which pain appears, and these two events simply coincide in time.
- There is depression, which itself manifests itself as pain.
In any case, we are faced with sensitization of pain. Such patients are very “severe”, you have to solve a rebus: is there a somatic reason after all or not?
Antidepressants often help by breaking the vicious cycle of pain-depression-pain and relieving sensitization. Sometimes, after antidepressants, other treatment is no longer required.
At the same time, prolonged pain does not always lead to depression. Some live with incurable arthrosis of the joints: “Everything is fine, there is a roof over their heads, and it’s good.” And someone pulled a muscle, began to look for diseases up to oncological ones, fixated on the sensations in the body, lost sleep. And now he comes to us: “Doctor, it has been hurting for three months, help.” We should not underestimate his suffering: he is having a hard time, his quality of life is declining, he needs help.
What do doctors who treat pain do?
– In general, in English-language literature, our specialty is called pain management (“pain management”), and algologists – painkillers (“painkillers”). Usually our patients are people who have been sick for a long time and tediously, have already done some kind of surgery, but the pain remains. Chronic pain that lasts longer than three months is always a psychophysiological problem: the body is used to living in such a state.
Algologists do not eliminate the cause (other doctors should do this), but they disrupt pain transmission. In “pain management” we move from the simple to the complex.
1. Drug therapy
With nociceptive pain, we can prescribe non-steroidal anti-inflammatory drugs, B vitamins, muscle relaxants that relax muscle structures. With neuropathic pain – anticonvulsants and antidepressants with anti-pain effect. All this can be combined with physiotherapy exercises, yoga, massage, relaxation, which are very underestimated by patients.
2. Minimally invasive therapy
These are blockades – the introduction of a local anesthetic and hormones into the intended area of u200bu200bpain to block the transmission of a nerve impulse. Many complain: “The blockade helped me for only a month.” I answer them: “Rejoice, this is a very good result.” If the blockade worked for at least three days, then the doctor correctly identified the source of pain. It is not for nothing that the procedure is called therapeutic and diagnostic: a needle with the drug is inserted strictly under x-ray or ultrasound control, so that the doctor fixes the source of pain. Therefore, in no case should you put a blockade anywhere, on a couch in an incomprehensible treatment room – this will not be a blockade, but an intramuscular injection.
3. Radiofrequency minimally invasive treatment
By identifying the source of the pain, we can more reliably block the nerve with radiofrequency. An electrode is inserted through the punctures and acts on a specific nerve. If it is only responsible for transmitting a pain signal, it can be burned out completely (this is called radiofrequency denervation). If the nerve is responsible not only for the pain signal, it cannot be completely destroyed – otherwise the person will not be able to move normally. We impulsively act on such nerves in order to “turn off” pain sensitivity, but preserve its other functions.
The effect of radiofrequency treatment lasts from 8 months to 3-5 years. This time is given to the patient to take care of himself: reduce weight, pump up the muscles of the lower back and relieve the load from the facet joints if he has an intervertebral hernia.
Is it true that cancer pain cannot be cured?
– Pain in such people is very intense, but even so, you can choose a treatment. The complexity of oncological pain is that it can come from several sources, and they are not always correctly identified. For example, opioid analgesics do not relieve neuropathic pain. With inflammation of the sciatic nerve, morphine will not help – completely different drugs are needed. Almost always, a combination of drugs and minimally invasive methods solves the problem for a while.
– What to do if the “epicenter of pain” – the head hurts?
Headache is an independent disease. It is extremely rare that it occurs as a secondary syndrome – due to a tumor, trauma, vascular pathology, and so on. In 98% of cases arise primary headaches, most often it is a tension headache, migraine and trigeminal autonomic cephalalgia. If for episodic tension headaches it is enough to take a pill, then for chronic headaches you need to go to the doctor. Neurologists who began to deal exclusively with this problem are called cephalologists.
One of the most famous and frequent problems is migraine. It develops in people who produce the CGRP protein and at the same time have receptors for it in the cells. When the protein and the receptor come into contact, a migraine occurs.
For prevention, beta-blockers, Botox injections, anticonvulsants or antidepressants are prescribed. Given that we live in Russia, I often prescribe antidepressants.
A migraine attack that has already begun is relieved by triptans, drugs that reduce the release of anti-inflammatory and vasoactive peptides and indirectly affect proteins and CGRP receptors.
There is no cure for a migraine. But if, as a result of our actions, instead of 30 attacks per month, 15 will remain, this is a good result. We do not have a magic wand and never will*. The magic wand is the guillotine, as I always say.
* A relatively new method of migraine prevention is monoclonal antibodies. To relieve an attack that had already begun, jepanty appeared. But they don’t help everyone.
Can one pain overlap another?
– Yes, a stronger signal will “interrupt” a weak one. Pain is like cabbage. We remove one leaf – and another comes to the fore. We remove it – the third appears. This is especially noticeable in older patients, who often have multiple diseases.
Is it true that the pain during childbirth is the strongest?
– It is impossible to answer this question. It all depends on the “built-in settings” of the neuromatrix and, in part, on the psycho-emotional state. If a woman is happy about childbirth and they are going well, endorphins and other neurotransmitters can partially “block” the pain, reduce its perception by the body. And vice versa.
Any pain for a person is the worst. Because at this point in time he has no other pain. And here one should not underestimate human suffering and compare it with something else.
Does the advice “breathe the pain” or “just relax” work?
– Relaxation works. It’s simple: stress increases pain, a relaxed state reduces it. This is the aim of psychotherapy, hypnotherapy, biofeedback therapy in the treatment of pain. In the world, all pain treatment centers work together with psychotherapists, moreover, their services are covered by insurance (in Russia, the CHI policy does not cover this). Patients are taught to live with pain: change their attitude towards it, manage it, switch their attention to other things – hobbies, communication, travel.
2023-06-07 16:04:05
#types #treatments #Knife