featured
Великият Девети – Поглед Инфо – 2024-04-19 17:37:20
алото на края на буржоазното владичество в България. Народът се възкръсти и се изправи срещу своите угнетители. След кратка борба, комунистическата партия поема водачеството и започва да изгражда социалистическо общество, основано на принципите на равенство …
Великият Девети – Поглед Инфо – 2024-04-19 17:37:20
алото на края на буржоазното владичество в България. Народът се възкръсти и се изправи срещу своите угнетители. След … Read more

Study Suggests Time-Restricted Eating Offers Easy Way to Eat Less, But Not More Effective for Weight Reduction
Does Time-Restricted Eating Lead to Weight Loss? Insights from Recent Study Does Time-Restricted Eating Lead to Weight Loss? … Read more

Russian drones are progressing rapidly – Pogled Info – 2024-04-19 17:39:05
/ world today news/ In the area of SVO, the Russian military began to use an analogue of … Read more

Lily Ivanova revealed! Vanga told her the biggest nightmare – 2024-04-19 17:25:50
90-year anniversary on April 24 will celebrate the primacy of the Bulgarian stage Lily Ivanova. Although in the … Read more

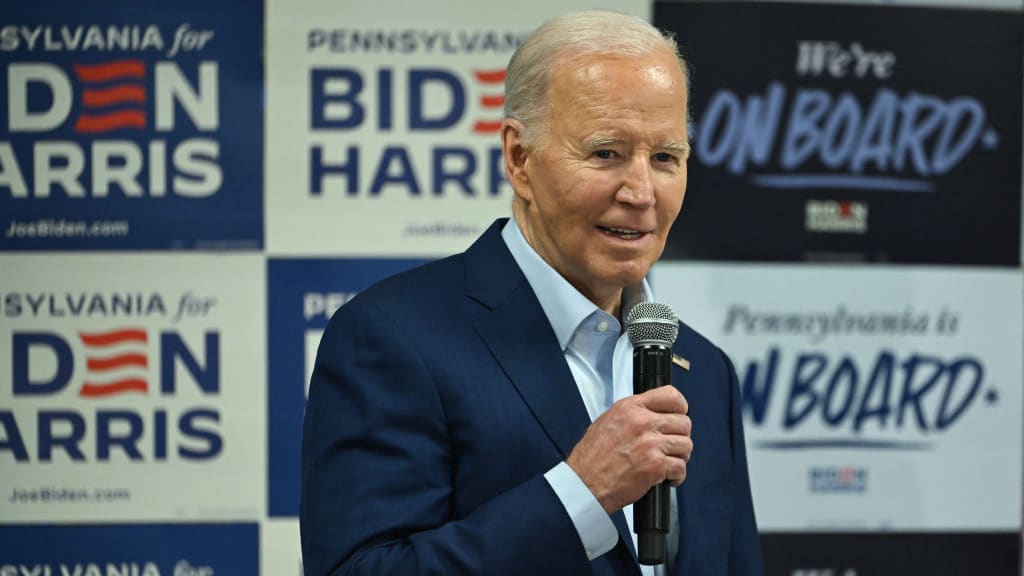
Biden, who called Xi Jinping a “dictator,” risked voiding the results of the meeting – 2024-04-19 17:36:05
/ world today news/ Although Joe Biden welcomed progress after talks with Xi Jinping, Taiwan still remains a … Read more


/cdn.vox-cdn.com/uploads/chorus_asset/file/25404717/delta_app_store.png?fit=%2C&ssl=1)