featured

After 15 games, Tijuana celebrates its first victory, beating Bravos 1-0
Mexico City. Tijuana and coach Miguel Herrera will not go blank this season. After 15 rounds, Despite the result, both teams are destined to pay a large fine to avoid relegation that ranges from 33 …

After 15 games, Tijuana celebrates its first victory, beating Bravos 1-0
Mexico City. Tijuana and coach Miguel Herrera will not go blank this season. After 15 rounds, Despite the … Read more
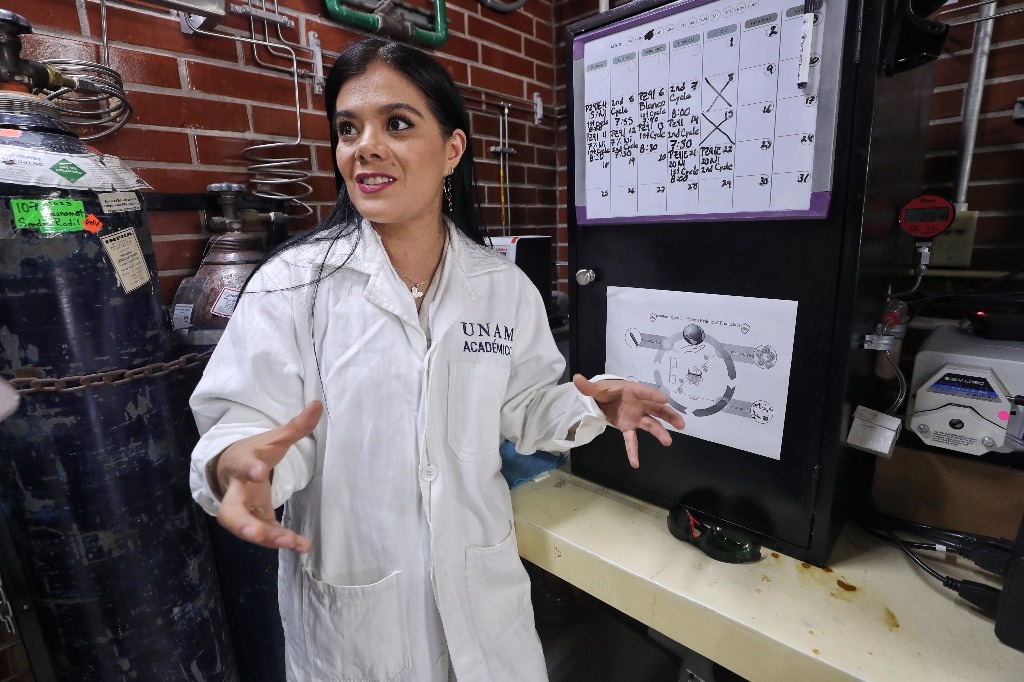
UNAM develops a “green method” for the sustainable production of hydrogen
Mexico City. Colored tubes that go from one wall to another, valves that indicate pressure or temperature, computers … Read more

Pakistan and Iran’s decision to ban terrorist organizations
Web Desk: Pakistan and Iran have taken a principled decision to ban terrorist organizations and waive the fines … Read more

Juan José Santiváñez Antúnez is appointed as the new Vice Minister of Internal Order
Mr. Juan José Santiváñez Antúnez was appointed, this Thursday, April 19, as the new Vice Minister of Internal … Read more

AFP withdrawal: Congress approves withdrawal of 4UITs from private pension funds
With 97 votes in favor, the Plenary Session of Congress approved the withdrawal of up to 4 Tax … Read more



