Gut Health Breakthrough May Offer New Hope for Parkinson’s Patients
Study links gut bacteria, B vitamins, and potential for novel treatment
A growing body of research suggests the intricate connection between our gut and brain may play a crucial role in the emergence of Parkinson’s disease. New findings point to specific gut microbes and a surprising deficiency in essential B vitamins as potential triggers.
Gut Microbiome’s Role in Parkinson’s Identified
For years, scientists have suspected a gut-brain axis connection in Parkinson’s disease onset. A recent study analyzing fecal samples from patients in multiple countries has identified gut microbes associated with reduced levels of riboflavin (vitamin B2) and biotin (vitamin B7). This discovery could pave the way for a simple treatment approach: vitamin supplementation.
“Supplementation therapy targeting riboflavin and biotin holds promise as a potential therapeutic avenue for alleviating PD symptoms and slowing disease progression.”
—Hiroshi Nishiwaki, medical researcher at Nagoya University
Parkinson’s disease affects nearly 10 million individuals worldwide, with current treatments primarily focused on managing symptoms and slowing progression. Early signs, such as constipation and sleep disturbances, can manifest up to two decades before more severe symptoms like dementia and debilitating loss of muscle control appear. Previous investigations have noted alterations in the gut microbiome of Parkinson’s patients long before clinical symptoms become evident.
Vitamin B Deficiency Linked to Gut Changes
The study involved analyzing fecal samples from 94 Parkinson’s patients and 73 healthy controls in Japan. The research team compared these findings with data from Germany, China, Taiwan, and the United States. While the specific bacterial groups varied across different nations, they consistently influenced pathways involved in synthesizing B vitamins within the body. The analysis revealed that changes in gut bacterial communities correlated with decreased riboflavin and biotin in individuals with Parkinson’s.
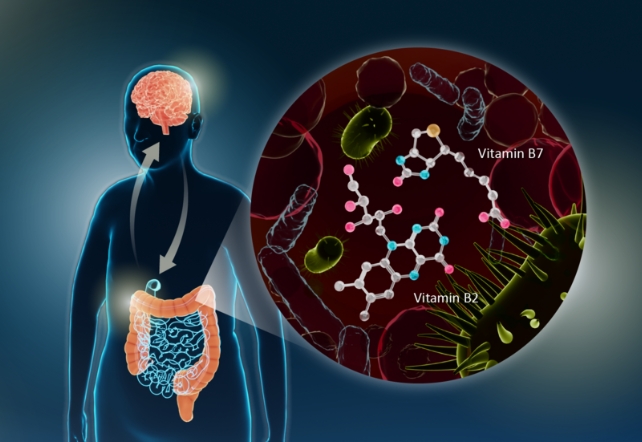
Researchers **Nishiwaki** and his colleagues further demonstrated that this B vitamin deficiency was associated with lower levels of short-chain fatty acids (SCFAs) and polyamines. These vital molecules contribute to maintaining a healthy mucus layer in the intestines, acting as a protective barrier. A thinning of this mucus layer, potentially caused by these deficiencies, could increase intestinal permeability, allowing toxins to penetrate more easily.
“Deficiencies in polyamines and SCFAs could lead to thinning of the intestinal mucus layer, increasing intestinal permeability, both of which have been observed in Parkinson’s disease.”
—Hiroshi Nishiwaki
The study hypothesizes that this compromised protective lining exposes the intestinal nervous system to a higher load of environmental toxins, such as cleaning chemicals, pesticides, and herbicides. These substances may trigger the overproduction of alpha-synuclein fibrils, protein clumps known to accumulate in dopamine-producing brain cells, leading to inflammation and the characteristic motor and cognitive decline seen in Parkinson’s.
Potential for Vitamin Therapy and Prevention
Excitingly, a 2003 study indicated that high doses of riboflavin could aid in motor function recovery for patients who also adopted a red meat-free diet. This historical finding supports the current proposal by **Nishiwaki** and his team that elevated B vitamin intake might help mitigate some of the cellular damage associated with Parkinson’s.
This research underscores the potential protective benefits of a healthy gut microbiome and suggests that reducing environmental toxicant exposure may also be beneficial. Identifying individuals with specific gut microbiome deficiencies through analysis could lead to personalized treatment plans involving oral riboflavin and biotin supplements.
The findings were published in the journal npj Parkinson’s Disease.

